KEY PAIN INDICATIONS
Many chronic conditions are challenging to manage. Here we focus on eight key pain conditions with a high unmet need among patients and/or healthcare professionals.
Our aim here is to provide the pain community with in-depth information about these conditions; from disease understanding to management approaches.
CHRONIC LOW BACK PAIN
Chronic low back pain (cLBP) is defined as pain in the lumbar back region that persists for 12 weeks or longer.1 It has many different causes, and often presents in a non-specific manner.1,2 cLBP represents a leading cause of disability, with a pronounced impact on quality of life, and major economic and societal consequences.2
Epidemiology
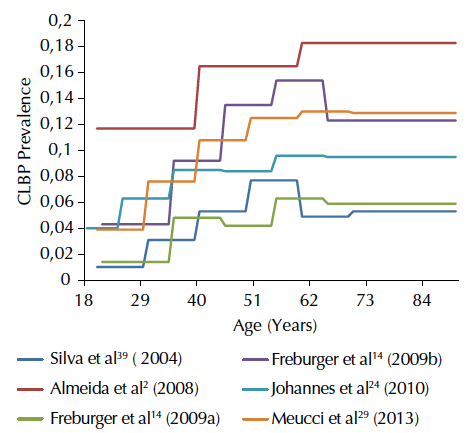
LBP represents a significant economic and social problem. From 2006 to 2016, the prevalence of both acute and chronic LBP has more than doubled.3 It is estimated that 11.9% of the global population suffers from LBP (either acute or chronic) at any point in time, rising to almost a quarter (23.2%) over any 1-month period.6 The prevalence of cLBP has been reported as 4.2% in people aged 24–39 years and 19.6% in those aged 20–59 years in two separate studies.7 Its prevalence continues to increase as the population ages, and both men and women in all ethnic groups are affected to a similar extent.3
Risk factors
There are a multitude of potential initiating factors described for LBP. However, many are difficult to interpret because of the high prevalence of back pain in the general population.1,2 Physical factors contributing to LBP include physical status, heavy lifting and, rarely, underlying conditions such as infections, tumours or kidney stones.1 Strong psychological factors also play a role in the development of back pain.2
Risk factors for developing LBP:1
- Age
- Fitness level
- Pregnancy
- Weight gain
- Genetics
- Occupational risk
- Mental health
- Backpack overload in children
- Underlying conditions
Causes
LBP represents a functional disorder that, in many cases, involves general degeneration of the spine associated with normal wear and damage as people age.1 Often, the exact aetiology of back pain remains unclear, leading to the majority of cases being labelled as ‘non-specific’.1,2 In cases where causes of back pain can be determined, they are mostly mechanical in nature, although these can also be a result of underlying conditions.1
Causes of specific low back pain1
| Mechanical causes |
|---|
| Sprains and strains |
| Intervertebral disc degeneration |
| Herniated or ruptured discs |
| Radiculopathy |
| Sciatica |
| Spondylolisthesis |
| Traumatic injury |
| Spinal stenosis |
| Skeletal irregularities |
| Serious underlying conditions |
| Infections |
| Tumours |
| Cauda equina syndrome |
| Abdominal aortic aneurysms |
| Kidney stones |
| Other underlying conditions |
| Inflammatory diseases of the joints |
| Osteoporosis |
| Endometriosis |
| Fibromyalgia |
Signs and symptoms
Traumatic or degenerative conditions of the spine are the most common causes of cLBP.1 Symptoms may include dull aching pain, sharp pain, tingling or burning, weakness of the legs or feet. The pain may be mild or it can be so severe that surgery is warranted, and flexibility may be lost permanently.1
Comorbidities associated with cLBP include a higher frequency of musculoskeletal and neuropathic pain conditions, sleep disturbance and mental health disorders such as anxiety and depression.8 Psychological factors play an important role in a patient’s ability to retain employment, and the financial burden on healthcare systems is enormous.2
Symptoms of cLBP may include:
- Pain
- Numbness
- Tingling sensations
- Spasms
- Muscle weakness
Pathophysiology
While cLBP often arises from a mechanical cause, neuropathic mechanisms play a part in most cases.1,5 Therefore, cLBP can be classified as a mixed pain syndrome.5
- Tissue injury with a subsequent inflammatory response usually leads to non-specific nociceptive pain.
- Neuropathic pain describes somatic referred pain originating from the lumbar spine and/or nerve roots (radicular pain/radiculopathy).
Studies have demonstrated that a large proportion of patients (20–55%) with cLBP have a higher than 90% likelihood of a neuropathic pain component, which is also suspected in a further 28% of patients.5 Such presence of a neuropathic pain component is associated with more severe pain symptoms and higher healthcare costs.5
Qualities and descriptors of neuropathic vs nociceptive pain5
| Neuropathic | Nociceptive | |
| Main characteristics | Maladaptive and chronic in nature | Short-lived response, adaptive, with resolution upon healing of injury. Some inflammatory hyperalgesia may also be present, as is the case with neuropathic pain |
|---|---|---|
| Qualitative description of pain | Paroxysmal (e.g. electrical shock-like pain, stabbing or shooting); abnormal thermal sensations (e.g. extreme cold or burning). Its occurrence may be spontaneous, or because of non-painful stimuli such as moderate heat or cold (allodynia), light touch or an exaggerated response to painful stimuli (hyperalgesia) | Dull or aching throbbing |
| Cause | Pain that is a consequence of a lesion or disease affecting the somatosensory system, e.g. mechanical nerve root compression, local nerve fibre damage, inflammatory mediators arising from a degenerated disc on nerve fibres | Tissue damage, tissue-damaging stimuli, inflammation |
Diagnosis
Back pain starts as acute pain and, aside from the initial cause, peripheral/central sensitisation contributes to the progression of acute to chronic pain.3 Depending on when a patient presents to a physician, back pain may be diagnosed as acute or chronic. A complete medical history and physical examination will be conducted to identify any serious conditions causing LBP, and imaging – while not usually warranted – may be utilised to rule out specific causes of pain such as tumours and spinal stenosis.1 Despite the various tests and examinations carried out, it is difficult to ascertain the exact cause of cLBP.
- X-rays
- Ultrasound imaging
- Bone scans
- Blood tests
- Electrodiagnostics
- Magnetic resonance imaging
- Discography
- Computed tomography
- Myelograms
Management
To guide the choice of treatment, clinicians should investigate the mechanisms underlying the pain.9 As the cause of cLBP can be diverse and multifactorial, determining the pain mechanism may allow for targeted treatment.10,11 However, identifying the pain mechanism based on patient phenotype remains a considerable clinical challenge.10
Mechanistic treatment of cLBP11
| Drug class | Effective in nociceptive pain | Effective in neuropathic pain | Effective alone in neuropathic cLBP | Effective in combination in neuropathic cLBP |
| Paracetamol | ✓ | ✕ | ✕ | ✓ with tramadol |
| NSAIDs | ✓ | ✕ | ✕ | ✓ COX-2 with pregabalin |
| Opioids | ✓ | ✓ | ✓ for tapentadol (lack of adequate studies for other opioids in cLBP) | ✓ Buprenorphine with pregabalin |
| Antidepressants | ✕ | ✓ | ✓ | for duloxetine (no clear evidence/ conflicting data†) |
| Anticonvulsants | ✕ | ✓ | ✕ | ✓ with COX-2 or with opioid |
| Topical lidocaine/ capsaicin | ✕ | ✓ * | ✓ for lidocaine and capsaicin |
effective; not effective.
*No label; †See Urquhart DM et al. Cochrane Database Syst Rev. 2008;(1):CD001703.
cLBP: chronic low back pain; COX-2: cyclooxygenase-2; NSAID: non-steroidal anti-inflammatory drug.
A range of strategies can be used to manage cLBP. This includes non-pharmacological and pharmacological as well as surgical treatments.1,2,9 Current treatment guidelines and recommendations include non-pharmacological management, such as hot or cold packs, physical activity to strengthen muscles and medications.1 Acute pain is often temporarily relieved by drugs, though this may not be sufficient to achieve sustained pain relief in the case of cLBP.2 Commonly used medications include non-opioid analgesics, such as paracetamol/acetaminophen and non-steroidal anti-inflammatory drugs, or opioids.2
The latest European Pain Federation position papers are available here: https://europeanpainfederation.eu/advocacy/position-papers/
Treatment options for cLBP1,2,9
| Conventional treatments |
| Hot or cold packs |
| Activity |
| Strengthening exercises |
| Physical therapy |
| Traction |
| Medicines |
| Analgesic medications |
| NSAIDs |
| Opioids |
| Anticonvulsants |
| Antidepressants |
| Counterirritants |
| Non-surgical procedures |
| Spinal manipulation and spinal mobilisation |
| Acupuncture |
| Biofeedback |
| Nerve block therapies |
| Epidural steroid injections |
| Transcutaneous electrical nerve stimulation |
| Surgical procedures |
| Vertebroplasty and kyphoplasty |
| Spinal laminectomy |
| Discectomy or microdiscectomy |
| Foraminotomy |
| Intradiscal electrothermal therapy |
| Nucleoplasty (plasma disc decompression) |
| Radiofrequency denervation |
| Spinal fusion |
| Artificial disc replacement |
NSAID: Nonsteroidal anti-inflammatory drug.
Unmet needs
A major unmet need for patients with cLBP is attaining knowledge of the source of pain. Recent guidelines state that clinicians who see patients with cLBP should explore the mechanisms that underlie the acute/chronic pain.9 This would allow for the use of more tailored therapy to optimise outcomes for the patient and avoid the generalised diagnosis of LBP that may lead to poor treatment. However, the large number of possible physical and non-physical causes of cLBP makes this difficult. In some instances of cLBP, multiple pain generators can work together; in such cases, multidisciplinary diagnosis and multimodal treatment options can be of use.5,12
Click here to register for CHANGE PAIN® and access in-depth educational resources on chronic low back pain. CHANGE PAIN registration page